How will pregnancy and birth change my body? This is one of the big questions EVERYONE asks. This is a fair question because although it is a natural process, we aren’t meant to “bounce back” to the way we were before.
Having a baby changes you permanently and can leave you with side effects or injuries. In fact, some issues are so common that they are overlooked as a “necessary evil” such as incontinence (lack of control over your bladder or bowels). It’s crucial to have the right tools and know-how to navigate your postpartum period for a lifetime of health. Here are some of our top suggestions…
Access to Knowledge

The first thing on our list of postpartum necessities is access to knowledge. Give yourself several credible and evidence-based resources for information. There are many great books out there, or sign up for a free copy of our Hair to Toe Guide.
There you can find out what postpartum symptoms are normal, common, exist on a spectrum, or should have a doctor’s opinion.
There is no substitute for the advice of your trusted doctor. Postpartum groups, friends, and your doula can all have great insight too. Just remember, everyone’s experience is different, you are an individual with a unique body and medical history.
Physical Therapy

You may never look or feel like you did before pregnancy, and that’s ok! You just went through something HUGE. The important thing is to feel healthy, capable, and pain-free. Physical therapy is something to consider to help pelvic weakness, back pain, separated abdominal muscles, pelvic girdle pain, incontinence, prolapse, sexual dysfunction, and more.
Check with your insurance provider to see if they will help cover your physical therapy. If you can’t get to a physical therapist, check with your doctor to see what at-home movements or exercises are safe for you. It’s a good idea to wear a support brace to help stabilize your core and protect you from injury. Never push yourself to the point of pain.
Pelvic Support Bracing

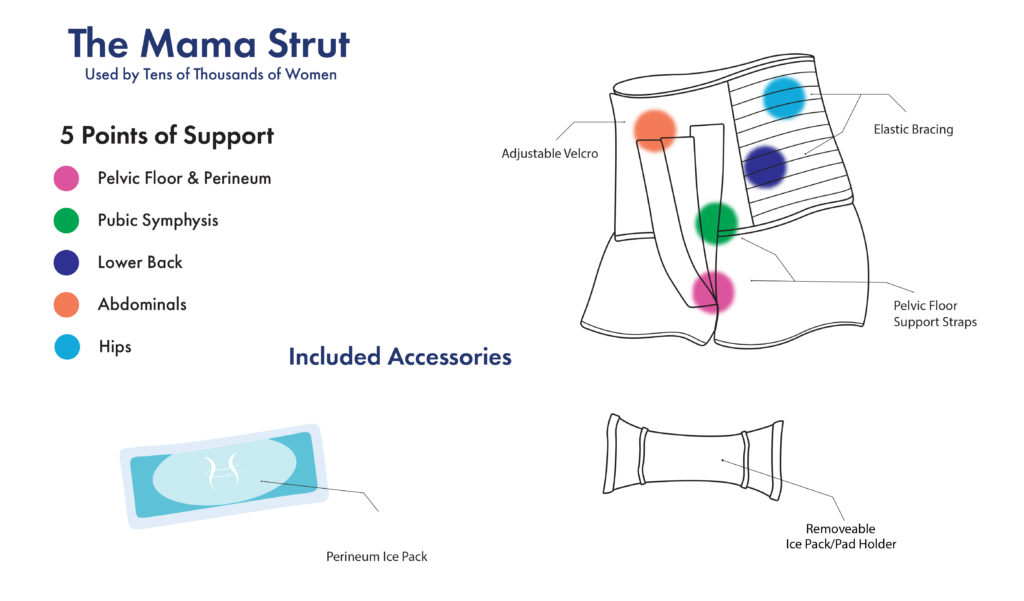
When you get hurt as an athlete, there’s a brace to help get you back in the game. There are ankle, wrist, shoulder, arm, knee, neck, and more braces! These braces can be used for compression therapy to ease pain and swelling, they support and protect the injured area, and they use what’s called optimal loading to gradually let your body do more work to return to normal function.
What about bracing for after having a baby?! We asked the same question before making the Mama Strut. Studies have shown that injuries sustained while pregnant and giving birth look similar to sports injuries. So throw away your girdles, corsets, and waist trainers. These are not built for health. The Mama Strut postpartum brace does everything the sports braces do, but it is specially designed for mamas and the issues they encounter!
Learn More
Ice and Heat Therapy

We won’t stop comparing athletes to mamas (because Mama, you are an athlete!). Let’s take another page out of the Sports Therapy Handbook. Ice and heat therapy has been around for centuries as an all-natural remedy to pain, swelling, and mobility problems.
Ice: Use right after giving birth (and any time after) on your perineum, abdominals, and lower back for instant pain and swelling relief.
Heat: Use after your swelling has gone down for pain relief, better mobility in muscles and joints, and to help with muscle spasms.
The Mama Strut pelvic bracing mentioned above comes with hot and cold packs that are easily insertable between your legs, on your tummy, and your back!
Postpartum Pads

We all know what period bleeding is like…your postpartum bleeding is NOT that. Your bleeding will last for weeks and you may see blood clots. You can’t use tampons and normal pads don’t usually cut it. Invest in postpartum pads built to stand up to the task. These will help you feel more comfortable and dry, giving you more time to focus on your baby and other things.
Check out Postpartum Pads
Stool Softener

Many mamas will feel constipated due to hormones, stretched muscles, anxiety, and vitamin supplements. It also may be painful to go to the bathroom because of tears, episiotomy, or hemorrhoids. You want to avoid straining too much at this time. A stool softener will help you pass your first movement and relieve some of the anxiety you may have about it. You should never try to hold back your bowel movements because it could end up being more uncomfortable in the end.
Getting exercise, eating right, and taking care of the area and any stitches you might have are also great ways to make things easier down there.
Perineal Spray or Wipes

There are many sprays and wipes that can help cool, soothe, numb, protect, and clean anywhere between your legs that may need it. These can be especially helpful before or after you go to the bathroom. Make sure you read the ingredients list, after all, this is going on and around one of the most sensitive areas on your body!
Peri Bottle

“Peri” refers to your perineum (the area between your vagina and anus). The peri bottle is just a squirt bottle you use before, after, or during your trip to the bathroom. Wiping with toilet paper can cause friction, pain, and leave traces of itself behind. You will most likely be given a peri bottle at the hospital but you can find other bottles with various designs and features. Always use clean water, experiment with temperature, but don’t make it too extreme, and consider adding other safe liquids to the water like witch hazel.
We began by saying knowledge is key, and that is how we will end. Prepare for the postpartum period as much as you prepared for your pregnancy, your birth plan, and your baby!